The Importance of Early Detection in Treating Chronic Kidney Disease
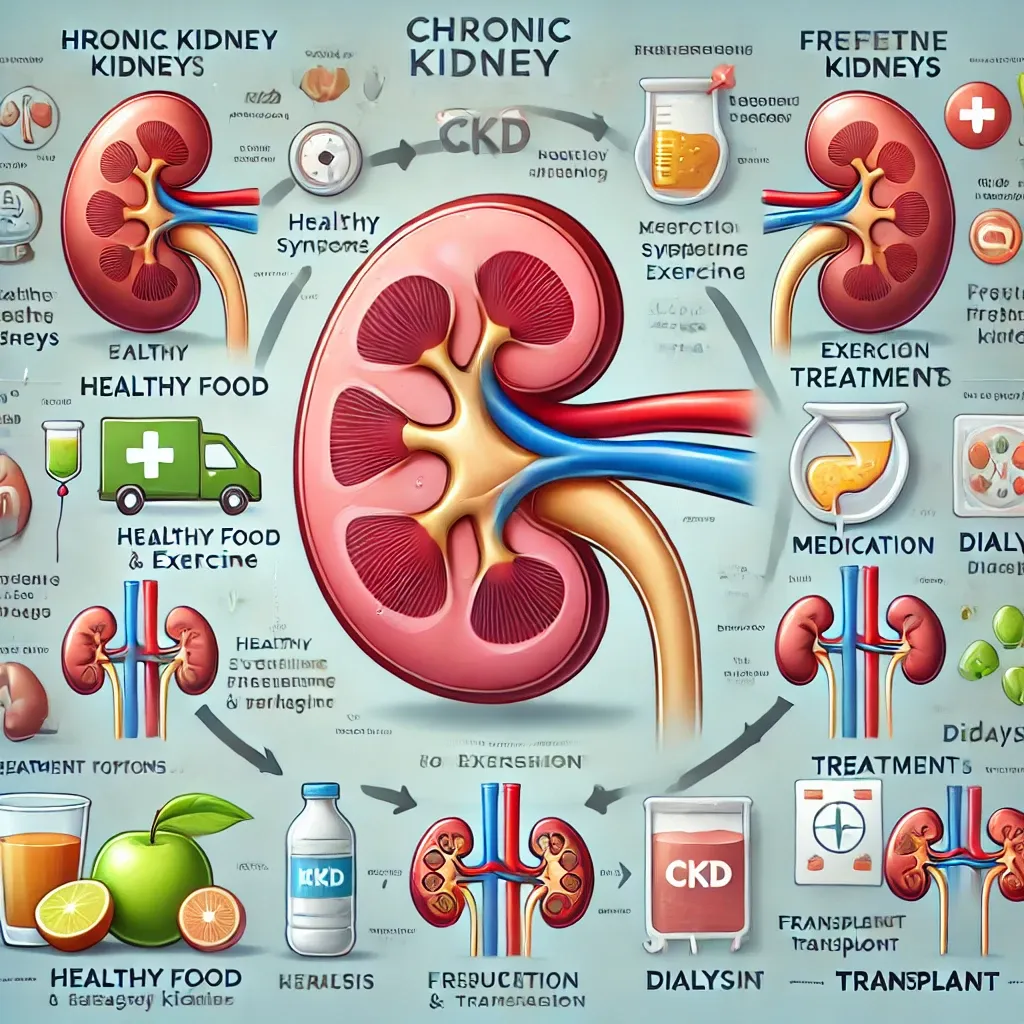
Chronic Kidney Disease (CKD) is a progressive condition where the kidneys lose their ability to filter waste and excess fluids from the blood. Identifying CKD early is crucial for slowing its progression and improving health outcomes. With timely care, people can manage the disease effectively and reduce the risk of severe complications.
Why Early Detection Matters
Detecting CKD in its early stages can significantly improve outcomes by enabling better management and preventing complications like kidney failure, heart disease, and other systemic problems. Early diagnosis allows healthcare providers to recommend lifestyle changes, medications, and treatments that slow disease progression. Because CKD often develops silently, regular screening is essential, especially for individuals at higher risk.
Early Signs of Chronic Kidney Disease
In its initial stages, CKD may not have noticeable symptoms, but some early warning signs include:
- Persistent fatigue and weakness.
- Swelling in the legs, ankles, or feet (edema).
- Frequent urination, especially at night (nocturia).
- Persistent itching.
- High blood pressure that is hard to control.
- Blood or protein in the urine, often identified during routine tests.
People with risk factors like diabetes, high blood pressure, heart disease, or a family history of kidney disease should prioritize regular health check-ups to monitor kidney function.
Stages of Chronic Kidney Disease
CKD is classified into five stages based on estimated glomerular filtration rate (eGFR), a measure of kidney function:
Stage 1: Kidney damage with normal or high eGFR (≥90 mL/min/1.73 m²). Symptoms may not appear, but managing underlying conditions is essential.
Stage 2: Mild reduction in eGFR (60-89 mL/min/1.73 m²). Lifestyle changes and monitoring become crucial.
Stage 3: Moderate reduction in eGFR (30-59 mL/min/1.73 m²). Symptoms such as fatigue and swelling may develop.
Stage 4: Severe reduction in eGFR (15-29 mL/min/1.73 m²). Intensive management and preparation for dialysis or transplant are necessary.
Stage 5: Kidney failure with eGFR (<15 mL/min/1.73 m²). Dialysis or a kidney transplant is required for survival.
Treatment Options for CKD
Although CKD has no cure, treatments can help manage symptoms and slow progression:
Lifestyle Changes
- Follow a kidney-friendly diet low in sodium, protein, and potassium.
- Maintain a healthy weight and engage in regular physical activity.
- Quit smoking and limit alcohol consumption.
Medications
- Blood Pressure Control: Medications like ACE inhibitors or ARBs help protect kidney function.
- Diabetes Management: Drugs to maintain healthy blood sugar levels.
- Supportive Treatments: Medications for anemia, bone health, or swelling.
Regular Monitoring
- Routine blood and urine tests track kidney health and detect changes early.
Advanced Treatments
- Dialysis: A procedure to remove waste and excess fluids when kidneys fail.
- Kidney Transplant: Replacing a damaged kidney with a healthy one from a donor.
Prevention and Proactive Care
Preventing CKD or slowing its progression requires managing key risk factors, such as high blood pressure, diabetes, and obesity. Regular screenings, early interventions, and adherence to treatment plans can make a significant difference in preserving kidney health.


